
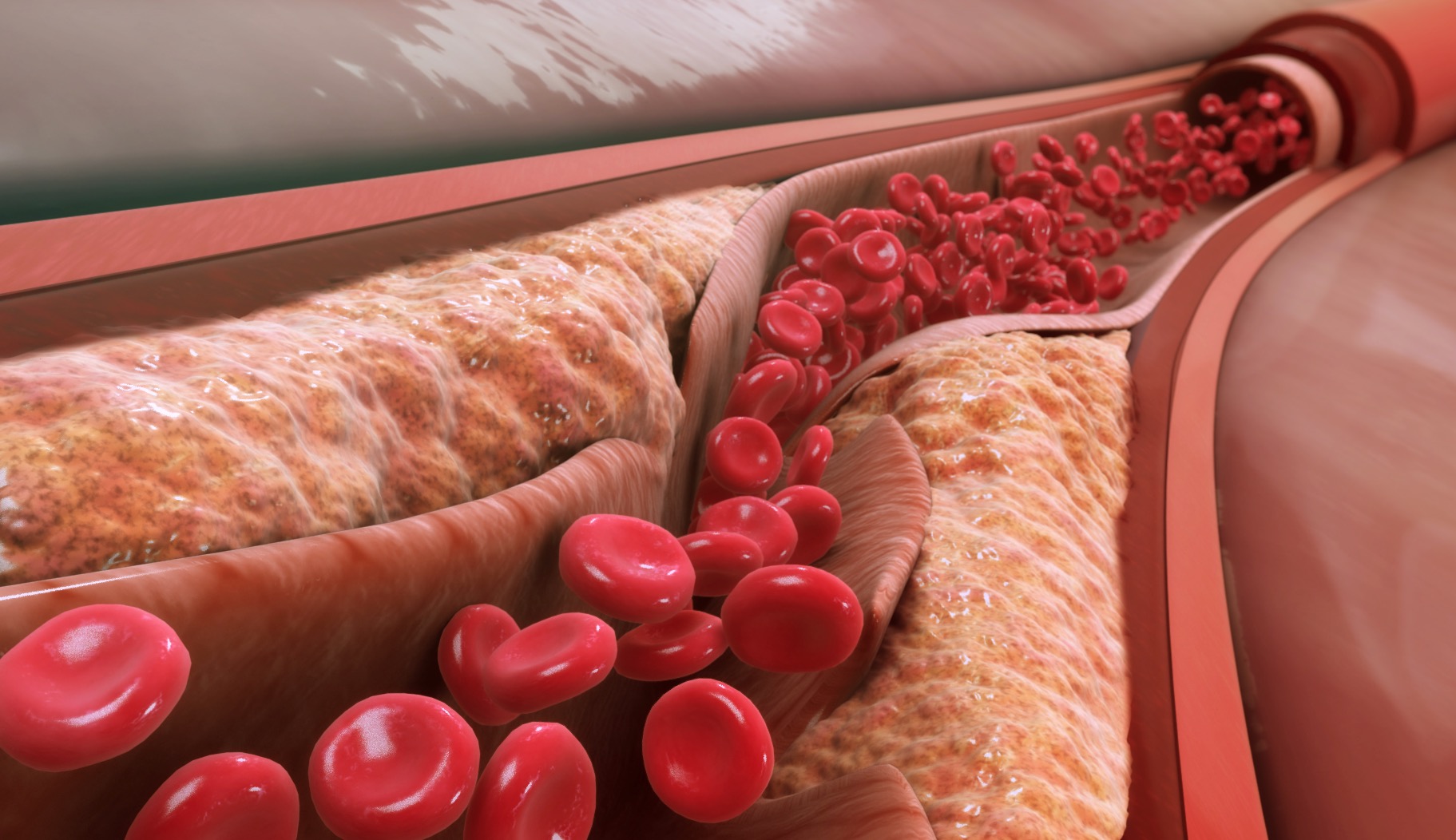
Tibial chronic total occlusions (CTOs) are among the most technically demanding challenges in peripheral intervention. These lesions are often long, calcified, and angulated—and yet they lie at the very heart of limb salvage efforts in patients with chronic limb-threatening ischemia (CLTI).
While recanalizing tibial CTOs may not offer the glamour of coronary work or aortic interventions, it is often what determines whether a patient walks or undergoes amputation.
In this post, we break down the strategies, tools, and practical pearls that help clinicians successfully cross and treat tibial CTOs.
Why Tibial CTOs Are So Challenging
Tibial CTOs often arise in patients with:
They’re usually:
Crossing is only part of the battle—creating a durable result that restores perfusion to the wound bed is the ultimate goal.
Step 1: Understanding the Anatomy
Pre-procedure planning is essential.
Imaging Essentials:
Clinical Tip: Always identify at least one target vessel with good distal outflow to the ulceration or amputation site.
Step 2: Crossing Techniques — Building Your Strategy
Progress gently; avoid forceful push that risks subintimal entry or perforation.
Subintimal techniques require finesse, especially in small-caliber tibials.
When antegrade fails, retrograde works:
Retrograde access requires precision and ultrasound guidance—but in expert hands, it dramatically increases CTO crossing success.
Step 3: Tools of the Trade
|
Tool |
Use Case |
|
Hydrophilic 0.014–0.018″ wires |
First-line crossing (Command, Pilot, Fielder) |
|
Support catheters |
CXI, Quick-Cross, Turnpike – essential for torque |
|
Reentry devices (limited tibial use) |
Off-label or specialized settings |
|
Micropuncture kits |
Pedal access and low-profile entry points |
|
Atherectomy |
For severe calcification prior to balloon angioplasty |
Always start with low-profile, highly steerable systems, and escalate only as needed.
Adjunctive Therapies After Crossing
Crossing is step one—definitive therapy requires durability.
Goal: Achieve direct flow to the angiosome of tissue loss. Revascularizing indirect vessels offers less wound-healing potential.
Success Metrics and Outcomes
Final Thought: Persistence with Precision
Tibial CTOs may test the patience and creativity of any operator. But for patients facing limb loss, crossing a 20 cm calcified artery may mean restoring life and mobility.
Success comes not from brute force, but from planning, finesse, and the willingness to try every pathway—antegrade, retrograde, subintimal, and beyond.
At TriVasc Academy, we advocate for a stepwise, anatomy-driven approach, supported by real-world case experience and advanced techniques—so more patients keep their limbs, and their independence.
Coming Soon at TriVasc Academy:
Pedal access masterclass videos
Tibial CTO algorithm cards
Angiosome-targeted revascularization planner
The content provided in this article and throughout the Trivasc Academy platform is intended for educational and informational purposes only. It does not constitute medical advice, diagnosis, or treatment, nor is it intended to replace the clinical judgment of qualified healthcare professionals. All clinical decisions—especially those concerning patient care, procedural planning, or surgical interventions—must be made by board-certified and appropriately credentialed medical practitioners based on their own professional expertise, institutional protocols, and applicable regional regulations.
While every effort has been made to ensure the accuracy, currency, and relevance of the information presented, Trivasc Academy makes no representations or warranties, express or implied, regarding the completeness, applicability, or clinical appropriateness of the content. We assume no responsibility or liability for any direct, indirect, incidental, or consequential harm, loss, or damage resulting from the use of any information or guidance provided herein.
Trivasc Academy does not endorse any specific device, technology, or clinical approach mentioned unless explicitly stated, and any reference to commercial products or services is for educational illustration only. Readers are strongly encouraged to consult official guidelines, product IFUs, and institutional policies before implementing any technique or procedure discussed on this site.
Use of this website and its content constitutes agreement to these terms. For full legal terms, please refer to our Terms of Use and Privacy Policy.
© 2025 TriVasc Academy. All content Copyrighted. All trademarks reserved.