
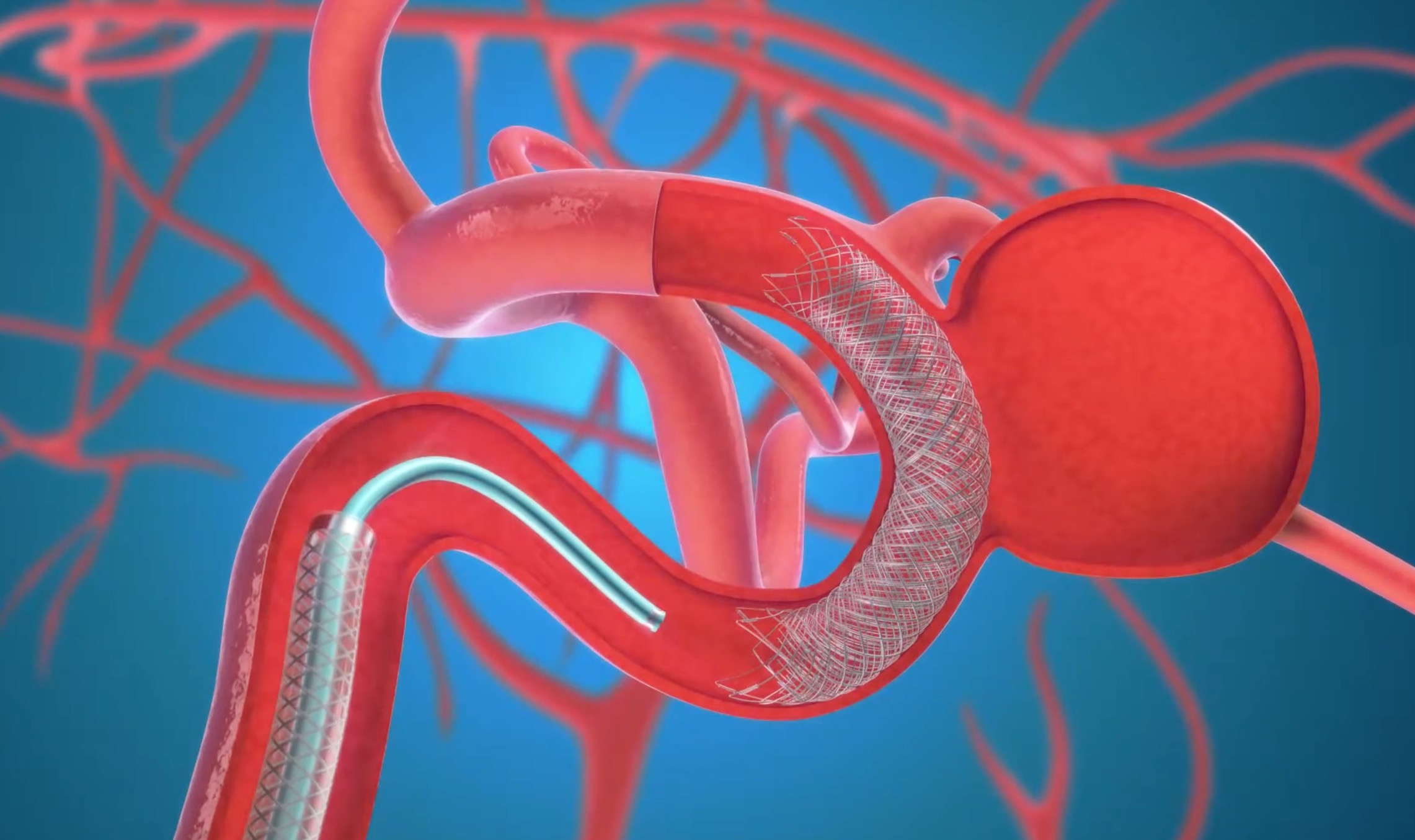
The evolution of neurointervention has revolutionized the treatment of intracranial aneurysms. Today, specialists are equipped with a growing arsenal of endovascular tools—from bare platinum coils to high-density flow diverters and intricate stent-assisted systems.
But with choice comes complexity. Particularly in complex aneurysms—those with wide necks, irregular shapes, fusiform morphology, or difficult locations—device selection becomes a critical determinant of both procedural success and long-term durability.
So how do we choose the right device for the right aneurysm, in the right patient, at the right time?
What Defines a “Complex” Aneurysm?
While definitions vary, complex aneurysms typically involve one or more of the following:
Each of these factors directly impacts device choice, access strategy, and long-term follow-up.
Device Options and Their Strategic Use
Let’s explore the most commonly employed endovascular approaches:
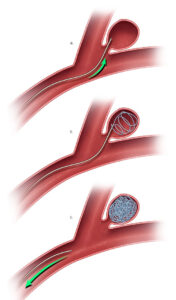
Best for:
Advantages:
Limitations:
Clinical tip: Coil compaction and recanalization remain risks, particularly in younger patients and high-flow locations.
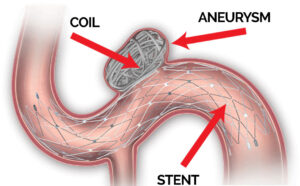
Best for:
Advantages:
Limitations:
Clinical tip: Closed-cell stents offer better coil containment; open-cell stents allow greater conformability in tortuous anatomy.
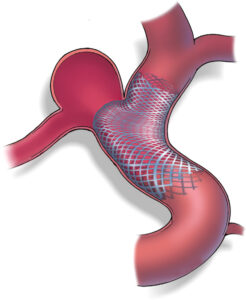
Best for:
Advantages:
Limitations:
Clinical tip: Always confirm vessel diameter and landing zones; ensure platelet function testing is optimized to reduce thromboembolic complications.
Choosing the Right Strategy: A Decision Framework
|
Aneurysm Type |
Preferred Approach |
|
Narrow-neck saccular (<7 mm) |
Simple Coiling |
|
Wide-neck bifurcation |
Stent-Assisted Coiling or Dual Stent Y-configuration |
|
Fusiform ICA aneurysm |
Flow Diversion |
|
Giant aneurysm |
Flow Diversion (± staged coiling) |
|
Posterior circulation aneurysm |
Coiling ± Stent-Assistance (Flow diverters with caution) |
|
Recurrent aneurysm |
SAC or Flow Diversion |
Patient factors such as age, platelet function, compliance with dual antiplatelet therapy, and comorbidities must always be part of the equation.
Adjuncts and Evolving Tools
Final Thought: Tailoring Tools to Anatomy
In complex aneurysm care, no single device is universally ideal.
Success lies in understanding aneurysm morphology, vascular geometry, hemodynamics, and the limitations of each tool in our hands.
Device selection is a strategic decision—not just about what can be deployed, but what will achieve the most complete, safe, and durable occlusion in that individual patient.
Because in the world of neurointervention, the difference between filling an aneurysm and fixing it — is the strategy behind the stent.
Coming Soon on TriVasc Academy
Device comparison charts, annotated case videos, and interactive 3D models for planning coil, stent, and flow diverter strategies.
The content provided in this article and throughout the Trivasc Academy platform is intended for educational and informational purposes only. It does not constitute medical advice, diagnosis, or treatment, nor is it intended to replace the clinical judgment of qualified healthcare professionals. All clinical decisions—especially those concerning patient care, procedural planning, or surgical interventions—must be made by board-certified and appropriately credentialed medical practitioners based on their own professional expertise, institutional protocols, and applicable regional regulations.
While every effort has been made to ensure the accuracy, currency, and relevance of the information presented, Trivasc Academy makes no representations or warranties, express or implied, regarding the completeness, applicability, or clinical appropriateness of the content. We assume no responsibility or liability for any direct, indirect, incidental, or consequential harm, loss, or damage resulting from the use of any information or guidance provided herein.
Trivasc Academy does not endorse any specific device, technology, or clinical approach mentioned unless explicitly stated, and any reference to commercial products or services is for educational illustration only. Readers are strongly encouraged to consult official guidelines, product IFUs, and institutional policies before implementing any technique or procedure discussed on this site.
Use of this website and its content constitutes agreement to these terms. For full legal terms, please refer to our Terms of Use and Privacy Policy.
© 2025 TriVasc Academy. All content Copyrighted. All trademarks reserved.