
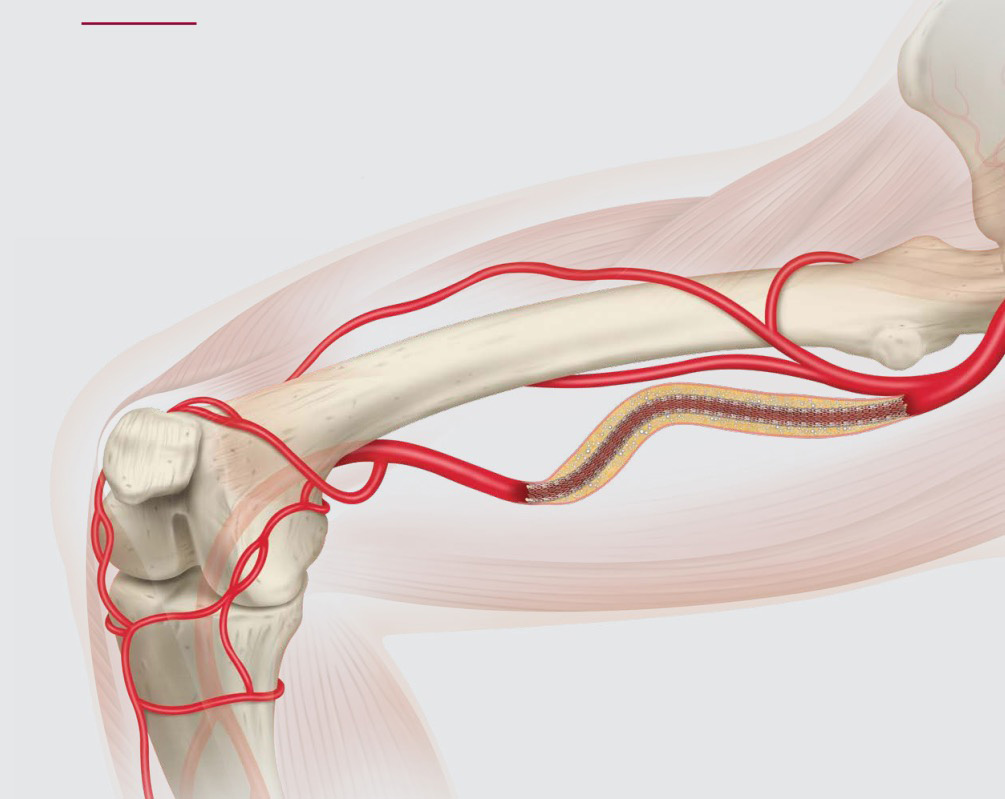
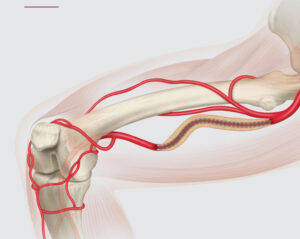
Peripheral artery disease (PAD) in the femoropopliteal segment is a common and increasingly complex challenge for interventionalists worldwide. When lesions span 15 cm, 25 cm, or even longer, durability—not just technical success—becomes the key goal.
While short focal stenoses may be treated with balloon angioplasty or spot stenting, long-segment disease in the superficial femoral artery (SFA) and popliteal artery requires a carefully considered strategy—one that accounts for mechanical forces, vessel behavior, and long-term patency.
This blog explores best practices for treating long femoropopliteal lesions, grounded in evidence and real-world experience.
What Makes Long Lesions Unique?
The SFA and popliteal artery are exposed to constant compression, elongation, torsion, and flexion, especially across the adductor canal and knee joint. These biomechanical demands make long lesions especially vulnerable to:
The longer the lesion, the greater the challenge in maintaining long-term success.
Strategy Begins With Preparation
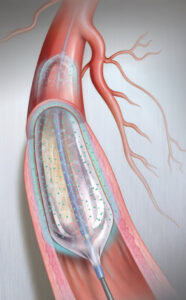
Before selecting a device, adequate vessel preparation is critical—especially in long lesions with calcification or occlusion.
Key Elements of Preparation:
Clinical tip: Don’t rush to treat—vessel prep defines the success of your definitive therapy.
What’s the Best Definitive Therapy?
Here’s how common treatment options compare in long lesions:
Pros:
Cons:
Ideal in patients with inflow/outflow disease already addressed, and in-stent restenosis cases.
Pros:
Cons:
Best suited to moderately long lesions with straight vessel segments and no calcium overload.

Pros:
Cons:
Excellent choice for focal or mid-length SFA disease in high-risk restenosis patients.
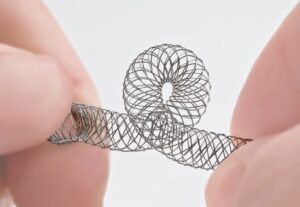
Pros:
Cons:
Preferred in long or severely calcified lesions, especially in mobile segments.
Pros:
Cons:

Reserved for long occlusions and restenosis after prior interventions.
What Does the Data Say?
Putting It All Together: A Practical Algorithm
|
Lesion Length |
Strategy |
|
<10 cm |
DCB alone or DES |
|
10–20 cm |
DCB + spot stent / IWS |
|
>20 cm |
IWS or Covered Stent ± Atherectomy and vessel prep |
|
CTO / heavily calcified |
Atherectomy + IWS or Covered Stent |
|
ISR or edge restenosis |
DCB or DES |
Always tailor therapy to anatomy, vessel dynamics, and reintervention options.
Final Thought: Think Long, Not Just Long Lesions
Every treatment choice in the femoropopliteal segment must anticipate future events: restenosis, access, reintervention, or patient lifestyle.
Durability isn’t just about patency—it’s about planning.
At TriVasc Academy, we emphasize evidence-based decision-making, lesion preparation, and device familiarity to build sustainable outcomes—not just short-term success.
Coming Soon on TriVasc Academy:
Femoropopliteal device comparison chart
Interactive lesion assessment guide
Case-based workshops on long-segment interventions
The content provided in this article and throughout the Trivasc Academy platform is intended for educational and informational purposes only. It does not constitute medical advice, diagnosis, or treatment, nor is it intended to replace the clinical judgment of qualified healthcare professionals. All clinical decisions—especially those concerning patient care, procedural planning, or surgical interventions—must be made by board-certified and appropriately credentialed medical practitioners based on their own professional expertise, institutional protocols, and applicable regional regulations.
While every effort has been made to ensure the accuracy, currency, and relevance of the information presented, Trivasc Academy makes no representations or warranties, express or implied, regarding the completeness, applicability, or clinical appropriateness of the content. We assume no responsibility or liability for any direct, indirect, incidental, or consequential harm, loss, or damage resulting from the use of any information or guidance provided herein.
Trivasc Academy does not endorse any specific device, technology, or clinical approach mentioned unless explicitly stated, and any reference to commercial products or services is for educational illustration only. Readers are strongly encouraged to consult official guidelines, product IFUs, and institutional policies before implementing any technique or procedure discussed on this site.
Use of this website and its content constitutes agreement to these terms. For full legal terms, please refer to our Terms of Use and Privacy Policy.
© 2025 TriVasc Academy. All content Copyrighted. All trademarks reserved.