

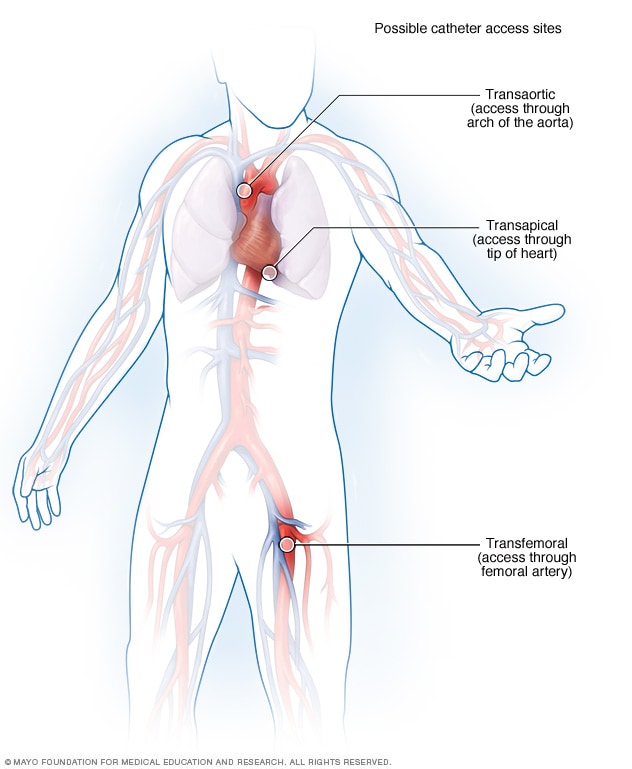
In the modern era of transcatheter aortic valve implantation (TAVI), access is everything. As device profiles shrink and indications expand to younger, lower-risk patients, the anatomical and technical complexities of vascular access remain one of the most critical—and underappreciated—determinants of procedural success and safety.
While transfemoral access remains the default for most TAVI procedures, many patients present with challenging iliofemoral anatomy, severe calcification, tortuosity, or previous vascular interventions that make the pathway far from straightforward.
This blog explores practical, case-based strategies for navigating these challenges, and when it may be time to switch to alternative routes.
Case 1: Severe Calcified Iliacs, Narrow Lumen
Scenario:
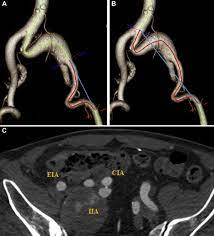
80-year-old female with symptomatic aortic stenosis. CTA reveals heavy bilateral circumferential calcification of common and external iliac arteries with minimal luminal diameter <5.5 mm.
Challenges:
Solution Options:
Clinical Tip: In patients with hostile iliacs, pre-procedural ballooning can sometimes create just enough room—provided the vessel is not brittle with concentric calcium.

Case 2: Tortuosity and Kinking in Pelvic Vessels
Scenario:
Male patient, 75, with known peripheral vascular disease. CTA shows severe S-shaped kinking of external iliac arteries bilaterally.
Challenges:
Solution Options:
Clinical Tip: Avoid over-rotating the delivery system in tortuous vessels—this increases the risk of arterial injury and embolization.
Case 3: Previous Aorto-Femoral Bypass Graft
Scenario:
A 78-year-old male with prior aorto-bifemoral bypass. No native access due to complete occlusion of native iliac vessels.
Challenges:
Solution Options:
Clinical Tip: Always perform a detailed CTA with 3D reconstruction in patients with prior vascular surgery. Understand the graft configuration thoroughly before choosing access.
Decision-Making Framework for Access Strategy
|
Anatomic Challenge |
Preferred Response |
|
Minimal femoral diameter <5.5 mm |
Low-profile system, pre-dilation, alternate access |
|
Severe iliac calcification |
Balloon pre-dilatation, consider transcaval |
|
Tortuous iliac arteries |
Buddy wire, stiff wire support, transaxillary |
|
Prior vascular grafts |
Transcarotid or direct aortic |
|
Aortic aneurysm or dissection |
Avoid transfemoral, consider axillary or apical |
|
Bilateral access not feasible |
Use single-side access with contralateral support |
Evolving Techniques & Tools
Beyond Anatomy: Patient-Centered Access Planning
Always consider:
A good access plan is not only anatomically feasible—it is procedurally safe, logistically realistic, and patient appropriate.
Final Thought: The Access Route Sets the Tone
A perfect valve deployment means little if the access fails.
Bleeding, dissection, and conversion to open repair all contribute significantly to morbidity in TAVI.
Great operators don’t just deploy valves—they build secure paths to get there.
At TriVasc Academy, we emphasize not only cutting-edge valve technologies, but also mastery of foundational access techniques. Because crossing the threshold safely is the first—and most crucial—step toward successful valve therapy.
Coming Soon on TriVasc Academy
Access planning checklists, CTA interpretation guides, and hands-on simulation modules for transfemoral, transcaval, and transaxillary approaches.
The content provided in this article and throughout the Trivasc Academy platform is intended for educational and informational purposes only. It does not constitute medical advice, diagnosis, or treatment, nor is it intended to replace the clinical judgment of qualified healthcare professionals. All clinical decisions—especially those concerning patient care, procedural planning, or surgical interventions—must be made by board-certified and appropriately credentialed medical practitioners based on their own professional expertise, institutional protocols, and applicable regional regulations.
While every effort has been made to ensure the accuracy, currency, and relevance of the information presented, Trivasc Academy makes no representations or warranties, express or implied, regarding the completeness, applicability, or clinical appropriateness of the content. We assume no responsibility or liability for any direct, indirect, incidental, or consequential harm, loss, or damage resulting from the use of any information or guidance provided herein.
Trivasc Academy does not endorse any specific device, technology, or clinical approach mentioned unless explicitly stated, and any reference to commercial products or services is for educational illustration only. Readers are strongly encouraged to consult official guidelines, product IFUs, and institutional policies before implementing any technique or procedure discussed on this site.
Use of this website and its content constitutes agreement to these terms. For full legal terms, please refer to our Terms of Use and Privacy Policy.
© 2025 TriVasc Academy. All content Copyrighted. All trademarks reserved.