
In the fast-paced world of neurointervention, the phrase “time is brain” is both a truth and a limitation. While rapid revascularization is essential in acute ischemic stroke, not all brains die at the same pace.
The critical factor behind this variability?
Collateral circulation.
As we refine our approach to mechanical thrombectomy and expand the window of intervention, understanding how and when collaterals compensate for arterial occlusion becomes central to patient selection, procedural planning, and long-term neurological outcomes.
What Are Collateral Pathways?
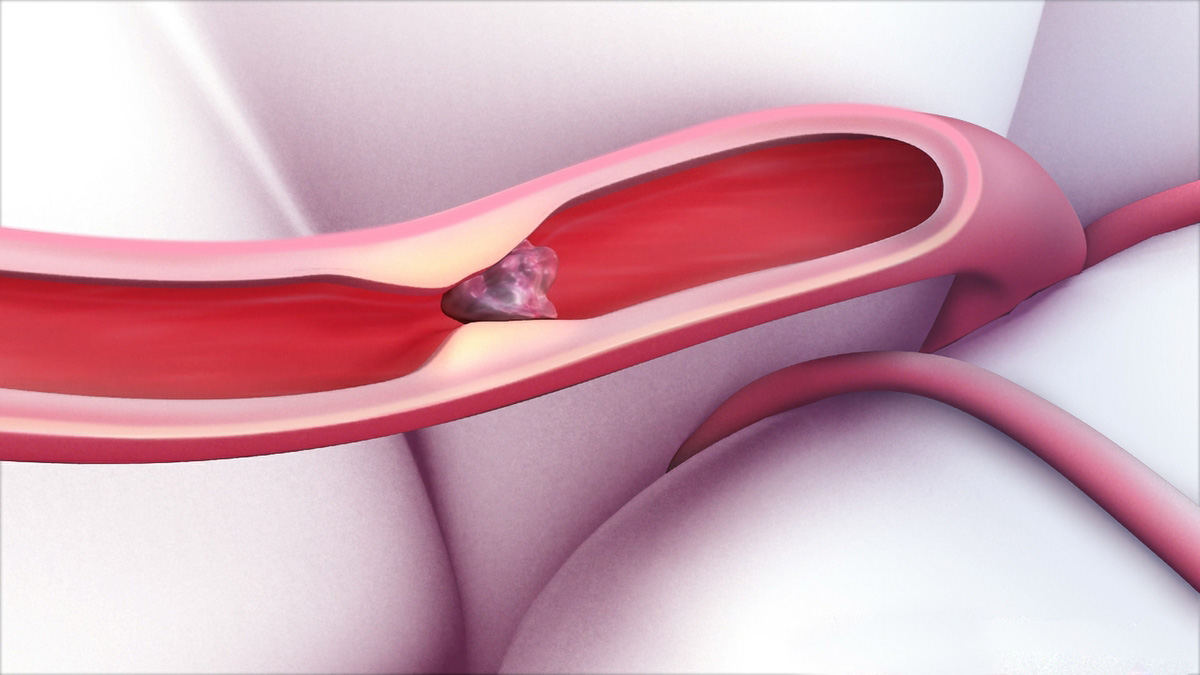
Collateral circulation refers to alternate routes of blood flow that bypass the primary site of arterial occlusion. In the cerebral circulation, these include:
These pathways act as biological buffers—delaying infarct progression and extending the ischemic penumbra’s viability.
Collaterals: The Real Clock Behind the Clock
Not all patients present equally. Two patients with the same MCA occlusion can have dramatically different outcomes:
The difference?
Patient B has robust collaterals.

This variability is why collateral quality is a key determinant in:
Assessing Collaterals in Real Time
Modern imaging allows rapid collateral assessment. Tools include:
CT Angiography (CTA)
Perfusion Imaging (CTP or MR-PWI)
Digital Subtraction Angiography (DSA)
Clinical Decision-Making: When Collaterals Inform Strategy
Understanding collateral status can guide:
Practical Considerations for Interventionists
Final Thought: We’re Not Just Reopening Arteries—We’re Preserving Viable Brain
Mechanical thrombectomy is not simply a race against time—it is a race against tissue loss.
Collateral circulation is the hidden variable that determines who has time—and who doesn’t.
By integrating collateral assessment into every step of stroke care—from imaging to the angio table—we can tailor interventions more wisely, select patients more ethically, and improve neurological recovery more meaningfully.
Because beyond the clot, there’s a network—silent, dynamic, and absolutely vital—that makes all the difference.
Coming Soon from TriVasc Academy:
Downloadable collateral scoring cheat sheets, imaging interpretation guides, and real case reviews highlighting the impact of collaterals on stroke intervention outcomes.
The content provided in this article and throughout the Trivasc Academy platform is intended for educational and informational purposes only. It does not constitute medical advice, diagnosis, or treatment, nor is it intended to replace the clinical judgment of qualified healthcare professionals. All clinical decisions—especially those concerning patient care, procedural planning, or surgical interventions—must be made by board-certified and appropriately credentialed medical practitioners based on their own professional expertise, institutional protocols, and applicable regional regulations.
While every effort has been made to ensure the accuracy, currency, and relevance of the information presented, Trivasc Academy makes no representations or warranties, express or implied, regarding the completeness, applicability, or clinical appropriateness of the content. We assume no responsibility or liability for any direct, indirect, incidental, or consequential harm, loss, or damage resulting from the use of any information or guidance provided herein.
Trivasc Academy does not endorse any specific device, technology, or clinical approach mentioned unless explicitly stated, and any reference to commercial products or services is for educational illustration only. Readers are strongly encouraged to consult official guidelines, product IFUs, and institutional policies before implementing any technique or procedure discussed on this site.
Use of this website and its content constitutes agreement to these terms. For full legal terms, please refer to our Terms of Use and Privacy Policy.
© 2025 TriVasc Academy. All content Copyrighted. All trademarks reserved.